Alzheimer’s disease research is at the forefront of innovative strategies to combat one of the most debilitating neurodegenerative diseases affecting millions of individuals. Neuroscientist Beth Stevens, based at Boston Children’s Hospital, has made significant strides in understanding the role of microglial cells, which act as the brain’s immune defense. Her findings suggest that these cells, while essential for maintaining neural health, can contribute to the progression of Alzheimer’s disease when they prune synapses excessively. The implications of her research could lead to groundbreaking treatments and earlier diagnoses for the 7 million Americans living with this condition, a number that is anticipated to double by 2050. As this research evolves, it stands on the shoulders of previous discoveries, underscoring the importance of curiosity-driven inquiries in the quest for the Nobel Prize in Medicine-level advancements.
The ongoing exploration into the mechanisms of Alzheimer’s disease is a pivotal area in neuroscience, shedding light on the intricate relationship between the brain’s immune cells and neurodegenerative disorders. Known as microglia, these specialized cells perform critical functions, including the cleanup of damaged neurons and maintaining healthy synapse formation. However, recent studies spearheaded by experts like Beth Stevens highlight a troubling aspect of their function, correlating abnormal activity with cognitive decline in conditions such as Alzheimer’s and others. This pursuit not only aims to innovate treatment methodologies but also strives to refine diagnostic markers for early detection of these debilitating disorders. Ultimately, the research journey emphasizes the value of foundational science in unraveling the complex pathways that influence brain health.
Understanding the Role of Microglial Cells in Alzheimer’s Disease
Microglial cells are a crucial component of the brain’s immune system, constantly monitoring for damage or disease. These cells play a significant role in maintaining brain health by clearing away dead neurons and modulating synaptic connections, which are essential for neural communication. However, recent research highlights that their functioning can go awry. Aberrant microglial pruning can lead to excessive synaptic loss, which is implicated in the progression of neurodegenerative diseases such as Alzheimer’s disease. Understanding how microglial cells contribute to these processes is fundamental to developing targeted therapies that aim not only to halt disease progression but to enhance cognitive function in affected individuals.
Beth Stevens, a prominent neuroscientist at Boston Children’s Hospital, has made significant strides in elucidating the relationship between microglial activity and Alzheimer’s disease. Her transformative research provides a new perspective on how these immune cells may contribute to the pathology of Alzheimer’s. Stevens’ lab has uncovered that improper pruning by microglia can exacerbate the accumulation of toxic proteins, a hallmark of neurodegenerative conditions. With a growing aging population, Stevens’ discoveries are pivotal in formulating preventative measures and therapeutic strategies that could reshape the future of Alzheimer’s treatment.
The Promise of Basic Science in Neurodegenerative Research
The journey of scientific discovery is often unpredictable, yet it is built upon foundational research that lays the groundwork for future breakthroughs. Beth Stevens emphasizes the importance of basic science in understanding complex diseases like Alzheimer’s. Her early work in neurobiology, particularly concerning microglial cell function, sets the stage for addressing broader questions in neurodegeneration. The support from organizations such as the National Institutes of Health has been foundational to these explorations, enabling researchers to create a comprehensive understanding of how immune responses in the brain are linked to diseases.
Stevens’ perspective on curiosity-driven research underscores a critical aspect of scientific advancement: innovations often arise from seemingly distant inquiries. While the exploration of a mouse’s visual system may appear disconnected from Alzheimer’s disease at first glance, these investigations yield insights that can lead to transformative therapies. The methodologies developed from foundational studies can lead to significant implications for treating human diseases, showcasing how basic science fuels the quest for cures. As scientists continue to delve into the intricate mechanisms underlying neurodegenerative diseases, the potential to discover novel disease-modifying treatments becomes ever more tangible.
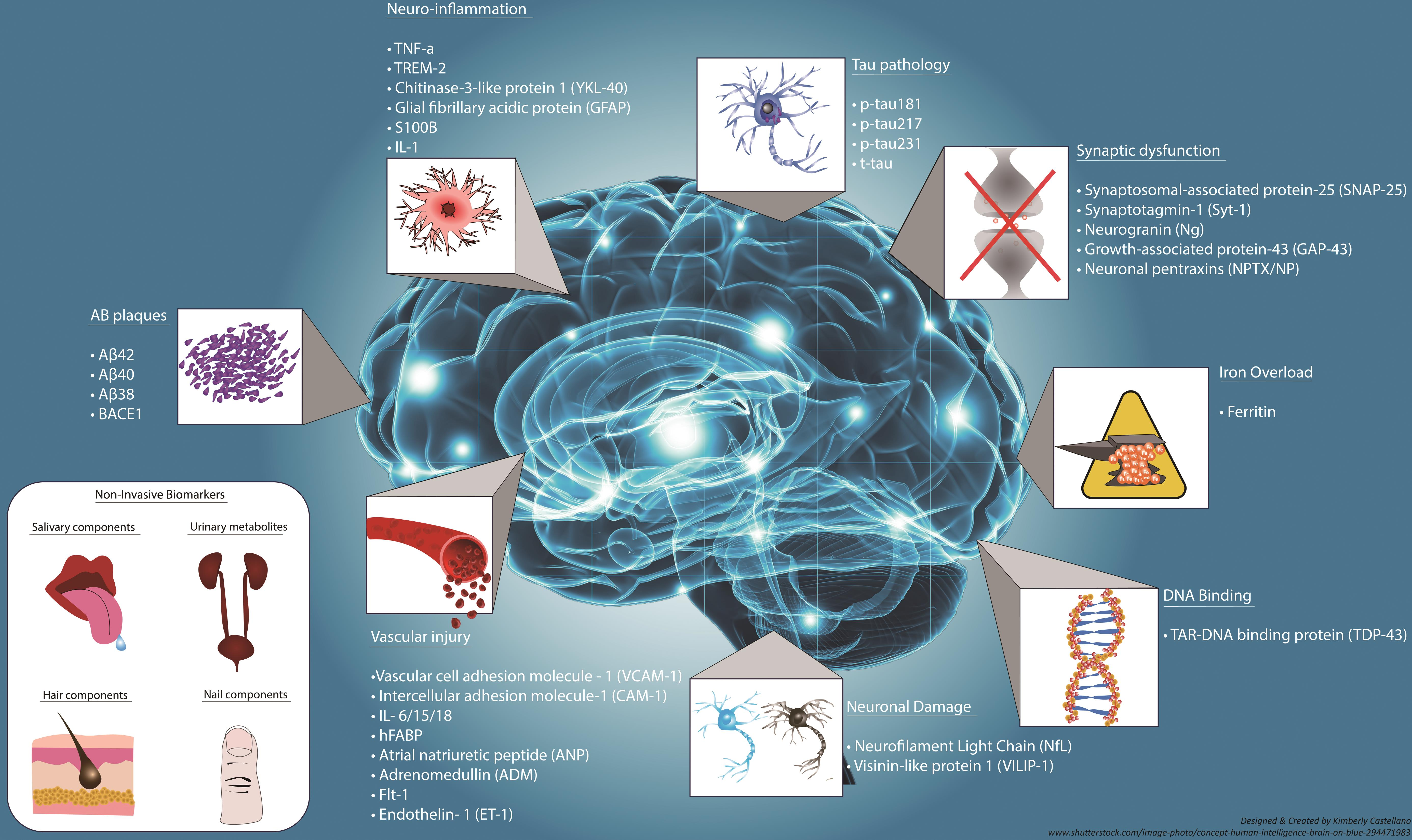
Innovations in Alzheimer’s Disease Biomarkers
Identifying reliable biomarkers for Alzheimer’s disease is crucial for early diagnosis and intervention. Innovative research by Beth Stevens and her team aims to discover new biomarkers that can signal the onset of Alzheimer’s before significant damage occurs. By investigating the molecular changes associated with microglial dysfunction, researchers hope to delineate specific markers that reflect the pathological processes at play in the brain. These biomarkers could drastically improve the ability to detect and treat Alzheimer’s disease in its nascent stages, potentially paving the way for interventions that significantly alter disease trajectories.
Moreover, the development of biomarkers can facilitate smoother clinical trials, allowing for a better selection of participants and more clearly defining the effectiveness of new therapies. As Stevens’ research progresses, it emphasizes a paradigm shift where early detection through such biological markers becomes a central theme in the ongoing battle against Alzheimer’s. The significance of establishing these connections not only highlights past research but also offers a promising outlook for future investigations aimed at alleviating the burdens associated with Alzheimer’s disease.
The Breakthroughs in Neurodegenerative Disease Research
Recent advancements in understanding microglial cells have positioned researchers like Beth Stevens at the forefront of neurodegenerative disease research. Her team’s groundbreaking work at the Broad Institute aims to redefine therapeutic approaches for Alzheimer’s disease, focusing on the mechanisms by which microglial cells operate. By shedding light on the dual role of microglia—both protective and potentially harmful—this research opens new pathways for developing effective treatments for Alzheimer’s and related disorders.
The potential to transform neurodegenerative disease treatment arises from a comprehensive understanding of underlying biological processes. Stevens’ work emphasizes not only the role of microglial cells in synaptic pruning but also their influence on overall brain health and function. As studies continue to evolve, there is hope for a new era in Alzheimer’s research that integrates insights from various fields within neuroscience, leading to more effective and targeted therapies that could alleviate the burden of neurodegenerative diseases.
Funding and Support in Alzheimer’s Disease Research
The role of federal funding in advancing Alzheimer’s disease research cannot be overstated. Organizations such as the National Institutes of Health have provided essential financial support to researchers like Beth Stevens, enabling groundbreaking explorations into the role of immunological factors in the brain’s environment. Such financial backing has proven crucial for sustaining long-term studies that foster significant scientific advancements. By investing in these explorations, government agencies bolster efforts to combat Alzheimer’s and other neurodegenerative diseases that affect millions.
Moreover, increasing public and private investment in Alzheimer’s research could lead to accelerated discoveries and a faster translation of scientific findings into clinical practice. The potential for developing impactful therapies relies heavily on consistent funding, which empowers scientists to pursue innovative research avenues. With the ongoing threat posed by aging populations, continued financial support for Alzheimer’s research promises new hope for prevention and treatment strategies, ultimately enhancing the quality of life for those affected by neurodegenerative diseases.
The Importance of Collaboration in Alzheimer’s Research
Collaboration across various research disciplines has emerged as a critical factor in effectively tackling Alzheimer’s disease. Scientists, clinicians, and institutions are increasingly coming together to share insights and methodologies, enhancing the overall understanding of neurodegenerative diseases. Beth Stevens’ work epitomizes the benefits of such interdisciplinary collaborations, especially at famed establishments like Boston Children’s Hospital and the Broad Institute. These interactions catalyze innovative approaches that can redefine treatment paradigms and inspire new therapeutic possibilities.
Moreover, collaborative endeavors can expedite the research process, allowing for faster identification of effective therapies. By pooling resources, expertise, and funding, research teams are better equipped to confront the challenges posed by Alzheimer’s. The synergy of collective efforts can lead to unexpected discoveries that may not occur in isolation, emphasizing the importance of a unified front in the battle against neurodegenerative diseases.
The Future of Alzheimer’s Disease Research
The future of Alzheimer’s research is brimming with potential, especially as the scientific community adapts to emerging technologies and novel methodologies. Techniques such as CRISPR gene editing and advanced imaging technologies are rapidly becoming integral tools for neuroscience researchers. Beth Stevens and her team are at the vanguard of utilizing these innovations in their research endeavors, which could lead to breakthroughs previously thought unattainable. Harnessing these technologies enhances the ability to dissect complex biological systems within the brain, shedding light on Alzheimer’s disease.
Furthermore, as awareness and urgency surrounding Alzheimer’s disease grow, the focus on finding effective solutions is amplified. Researchers are hopeful that the future will bring about a range of therapeutic options, including not only disease-modifying drugs but also lifestyle interventions and preventive measures. By fostering a prevention-oriented approach, scientists like Stevens are paving the way for a future where Alzheimer’s could be managed more effectively, significantly improving outcomes for individuals affected by neurodegenerative diseases.
Recognizing the Impact of Alzheimer’s on Society
The societal implications of Alzheimer’s disease are profound, affecting not only individuals but families and communities as well. As the Alzheimer’s Association estimates that the number of individuals with Alzheimer’s will surge, the associated caregiving and healthcare costs are expected to skyrocket. Researchers like Beth Stevens are aware of these challenges and are dedicated to finding solutions that not only address the disease at a clinical level but also consider its far-reaching impact on society. This holistic approach is vital in shaping research goals and inspiring interventions that comprehensively address the needs of patients and caregivers.
Furthermore, societal awareness plays a pivotal role in driving research funding and policy changes. As public understanding of Alzheimer’s disease grows, so does the urgency for innovative research and effective treatments. It is essential for society to acknowledge the scale of the challenge presented by neurodegenerative diseases, which in turn fosters a more informed and supportive environment for researchers to pursue their work. Moving forward, a concerted effort from all sectors will be vital to mitigate the effects of Alzheimer’s disease on individuals and society at large.
Personal Journeys in Alzheimer’s Research
Personal stories of researchers like Beth Stevens illuminate the profound commitment behind scientific exploration in Alzheimer’s disease. Beth’s path into neuroscience exemplifies the spark of curiosity that drives many scientists; her dedication stems from a desire to uncover the complexities of the brain and how they relate to diseases like Alzheimer’s. Such personal journeys not only humanize the quest for knowledge but also reflect the passion that fuels the fight against neurodegenerative disorders, inspiring future generations of scientists.
Sharing these personal narratives within the context of Alzheimer’s research can also inspire public engagement and support. By highlighting the stories of those dedicated to combating the disease, researchers contribute to a greater understanding and foster empathy for patients and their families. These narratives are essential in bridging the gap between scientific discovery and societal impact, reinforcing the idea that every advance made in research holds the potential to change lives fundamentally.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s disease research?
Microglial cells are crucial in Alzheimer’s disease research as they act as the brain’s immune system. They help clear out damaged cells and prune synapses, which are vital for neuron communication. However, abnormal pruning by microglia may contribute to Alzheimer’s and other neurodegenerative diseases, making them a significant focus of studies aimed at developing new treatments.
How has Beth Stevens contributed to our understanding of Alzheimer’s disease?
Beth Stevens has significantly contributed to Alzheimer’s disease research by transforming our understanding of microglial cells. Her work at Boston Children’s Hospital shows that aberrant pruning by these immune cells may lead to neurodegenerative diseases like Alzheimer’s. This research lays the groundwork for identifying new biomarkers and treatments.
What is the connection between neurodegenerative diseases and microglial cell function?
Neurodegenerative diseases, including Alzheimer’s, are linked to the improper functioning of microglial cells. These cells are responsible for maintaining brain health by removing damaged cells and regulating synapse pruning. When this process goes awry, it can contribute to disease progression, making microglia a focal point in Alzheimer’s disease research.
Why is funding important in Alzheimer’s disease research?
Funding is crucial in Alzheimer’s disease research because it supports the foundational science that leads to breakthroughs. For example, much of Beth Stevens’ work was driven by grants from the National Institutes of Health, which allowed for exploration into the roles of microglial cells in neurodegenerative diseases, paving the way for potential new therapies.
How is research on microglial cells influencing future Alzheimer’s treatments?
Research on microglial cells influences future Alzheimer’s treatments by identifying how these immune cells contribute to disease. Discoveries from studies led by scientists like Beth Stevens provide insights into the mechanisms of neurodegenerative diseases, leading to the development of new medications and early detection biomarkers.
What potential impact does Alzheimer’s disease research have on public health by 2050?
Alzheimer’s disease research, particularly the groundbreaking work on microglial cells, has the potential to significantly impact public health as the number of annual cases is expected to double by 2050. Effective treatments stemming from this research could alleviate the expected rise in healthcare costs associated with caring for the growing population of individuals with Alzheimer’s.
| Key Points | Details |
|---|---|
| Research Focus | Neuroscientist Beth Stevens studies microglial cells, which function as the brain’s immune system. |
| Microglia Function | They help clear dead or damaged cells and prune synapses that transmit information among neurons. |
| Implications for Alzheimer’s | Aberrant pruning by microglia is linked to Alzheimer’s disease and other neurodegenerative disorders. |
| Potential Impact | Stevens’ findings could lead to new treatments and biomarkers for Alzheimer’s, affecting 7 million Americans. |
| Funding and Support | Stevens’ research is largely supported by federal funding, particularly from the National Institutes of Health. |
| Future of Research | Continued basic science research is crucial for understanding diseases and developing effective treatments. |
Summary
Alzheimer’s disease research is making significant strides thanks to advancements in understanding the role of microglial cells by scientists like Beth Stevens. Her pioneering work highlights the importance of these immune cells in maintaining healthy brain function and their potential link to neurodegenerative diseases. As research progresses, the insights gained can pave the way for innovative treatments and early detection methods, ultimately transforming the care for millions affected by Alzheimer’s disease.