Pediatric brain cancer is a critical health issue that affects countless children and their families each year. In particular, gliomas, which are a type of pediatric brain tumor, are often treatable yet pose significant risks of recurrence. A recent Harvard study has highlighted the promising role of AI in cancer prediction, revealing that advanced algorithms can significantly enhance the accuracy of relapse risk assessments. By utilizing temporal learning in medicine, researchers have developed innovative methods to analyze multiple brain scans over time, leading to improved brain tumor treatment strategies. Understanding pediatric brain cancer and leveraging cutting-edge technology like AI is essential in ensuring better outcomes for children fighting this devastating disease.
Childhood brain tumors, particularly those classified as pediatric gliomas, represent a significant challenge within the realm of oncology. These tumors, while often manageable with surgery, can have unpredictable recurrence rates that complicate treatment and monitoring. Recent advancements in artificial intelligence (AI) have opened new avenues for glioma recurrence prediction, as researchers explore novel techniques to enhance diagnostic accuracy. The concept of temporal learning allows medical professionals to analyze a series of brain scans, improving brain tumor treatment outcomes. This multidimensional approach to cancer management emphasizes the importance of leveraging innovative technology to support the health and well-being of our youngest patients.
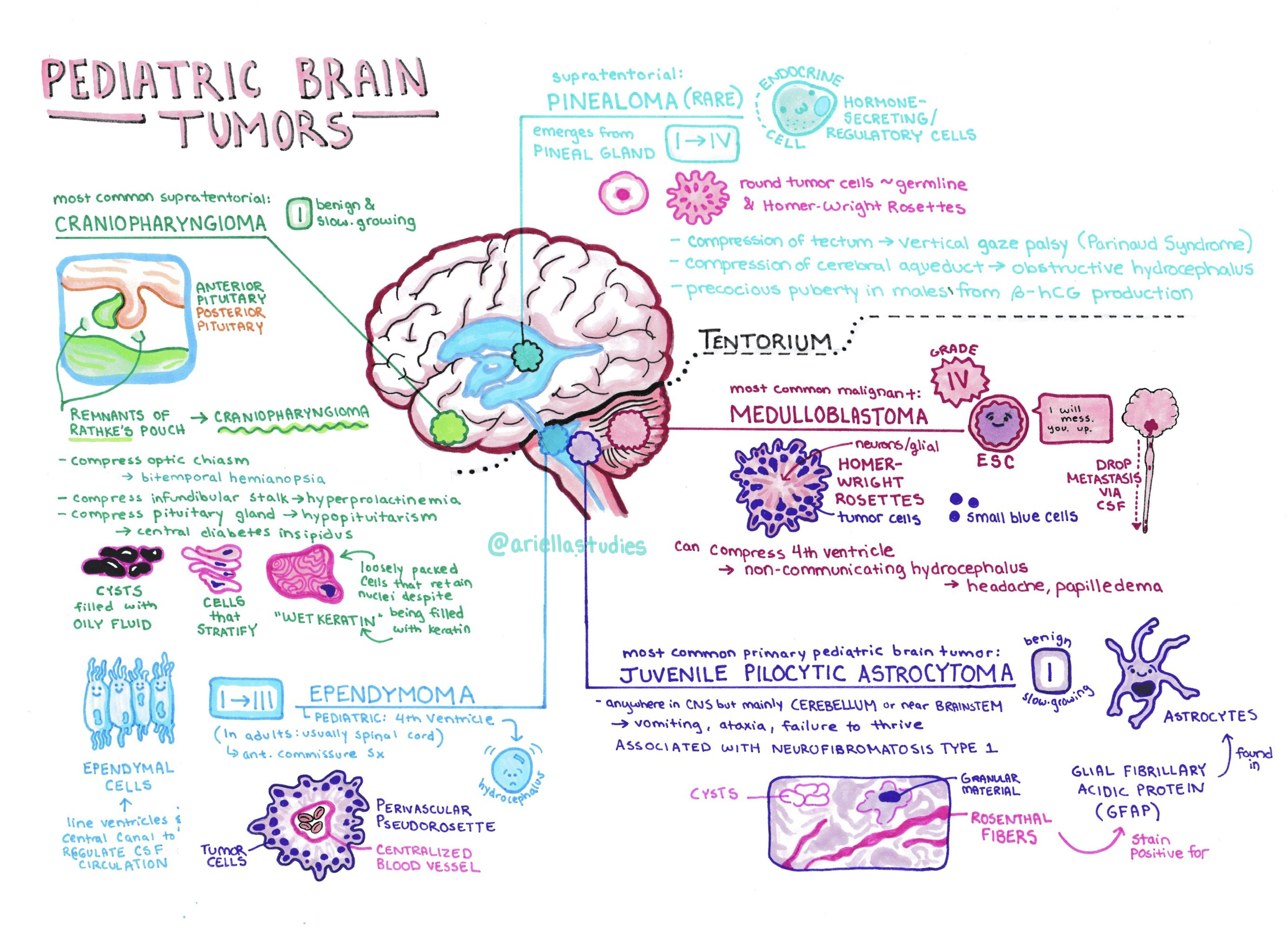
Understanding Pediatric Brain Cancer
Pediatric brain cancer, particularly gliomas, remains a significant concern within the medical community due to its complex nature and treatment implications. These tumors originate in the glial cells, which are crucial for supporting and protecting neurons in the brain. With advancements in medical imaging and treatment protocols, healthcare providers are increasingly focused on enhancing detection and prediction methods for the recurrence of these types of tumors. Given that pediatric patients often require long-term monitoring, understanding the risks associated with gliomas is essential for improving their health outcomes.
Treatment options for pediatric brain cancer have evolved alongside research developments. Surgery tends to be the first line of defense, with many pediatric gliomas proving curable through surgical resection alone. However, concerns about recurrence lead to ongoing studies aimed at optimizing post-operative care and surveillance strategies. Utilizing artificial intelligence (AI) tools significantly enhances prognostic capabilities, allowing physicians to predict which patients might face a relapse, ultimately leading to more tailored and effective treatment plans for these vulnerable patients.
The Role of AI in Predicting Glioma Recurrence
Artificial Intelligence has emerged as a powerful tool in the realm of cancer diagnosis and prognosis, especially in the context of gliomas. The recent study featured by Mass General Brigham highlights an AI model that employs temporal learning to analyze a series of magnetic resonance imaging (MRI) scans over time. This innovative approach allows for a more comprehensive review of changes in the tumor, significantly improving the prediction of recurrence risks compared to traditional single-scan evaluations. By analyzing patterns in multiple scans, the AI can detect subtle changes that may be indicative of an impending relapse.
The implications of AI-driven predictive models extend beyond mere diagnosis; they also promise to revolutionize treatment approaches for pediatric brain cancer. With accurate predictions of recurrence risk, doctors can strategize follow-up schedules and interventions more effectively, minimizing unnecessary imaging for low-risk patients while ensuring that those at higher risk receive prompt and appropriate treatment. This is particularly beneficial for children, who may experience anxiety and discomfort associated with frequent imaging sessions.
Temporal Learning in Medicine: A Breakthrough Approach
Temporal learning represents a groundbreaking methodology in medical AI, particularly for diseases characterized by complex progression patterns, such as pediatric brain cancer. Traditionally, AI models focused on individual images, which limited their ability to recognize evolving trends critical to patient outcomes. By leveraging temporal learning, researchers have initiated a paradigm shift that utilizes sequences of scans to inform predictions, providing a clearer picture of how tumors may change over time. This multi-scan approach enhances the predictive accuracy for glioma recurrence, offering substantial benefits in clinical decision-making.
The innovation behind temporal learning also facilitates a deeper understanding of patient-specific responses to treatment, allowing for personalized medical strategies. As shown in the study, this technique resulted in accuracy levels for recurrence predictions reaching an impressive 75-89%. Such insights can redefine how pediatric gliomas are monitored, leading to the potential for reduced imaging frequency and timely interventions tailored to individual risk profiles. Researchers are optimistic that these AI methodologies can be applied across various medical fields, paving the way for more refined predictive analytics in healthcare.
The Importance of Early Detection in Pediatric Brain Tumors
Early detection of pediatric brain tumors significantly influences treatment outcomes and patient survival rates. Many childhood cancers are curable, especially when identified and treated promptly. However, the recurrence of tumors like gliomas poses a considerable challenge, necessitating enhanced monitoring techniques over time. The integration of AI into early detection strategies not only improves the accuracy of ongoing assessments but also eases the burden on young patients and their families.
An AI-driven approach can streamline the follow-up process for patients previously diagnosed with pediatric gliomas, reducing the need for frequent imaging while ensuring that at-risk children receive vigilant care. This shift minimizes emotional stress for families and allows healthcare professionals to allocate resources more effectively. The ongoing collaboration between healthcare researchers and technology specialists is vital in keeping the focus on preventative care and early intervention to achieve better health outcomes for children battling brain cancer.
Advancements in Brain Tumor Treatment Protocols
The treatment landscape for pediatric brain tumors is continuously evolving, fueled by research advancements and technological innovations. In recent years, approaches to managing pediatric gliomas have shifted from conventional methods to more precise and individualized treatment protocols. Attuning to the unique biology of each tumor has enabled clinicians to optimize therapeutic efficacy while minimizing adverse effects, providing a better quality of life for young patients.
Current treatment protocols often involve a combination of surgery, radiation therapy, and chemotherapy. However, with the advent of AI-powered predictive modeling, treatment plans can be further refined. This personalization of care, driven by continuous analysis of imaging data and patient responses, may allow clinicians to implement timely interventions, such as adjuvant therapies, that can significantly alter disease trajectories. Furthermore, these advancements foster hope not only for improved survival rates but also for enhancing the overall well-being of children undergoing treatment for brain tumors.
The Impact of AI on Pediatric Glioma Management
The introduction of AI in managing pediatric gliomas marks a significant shift in how healthcare teams approach treatment and monitoring of brain tumors. By integrating AI tools into clinical practice, physicians can predict recurrence more accurately and tailor follow-up care based on individual risk assessments. This tailored approach has the potential to streamline patient care, reduce unnecessary stress for families, and ultimately lead to better health outcomes.
Moreover, AI’s role in pediatric glioma management extends beyond just prediction and immediate care. The data collected through the use of AI can inform future research directions, contributing to a deeper understanding of tumor behavior and response to different treatment modalities. As ongoing studies validate these models, the expectation is that AI will not only enhance current management practices but pave the way for revolutionary changes in the treatment paradigms for pediatric brain cancer.
Long-Term Implications of AI in Cancer Prediction
The long-term implications of employing AI in cancer prediction, specifically for pediatric brain tumors, can reshape the healthcare landscape. By consistently monitoring patient outcomes and refining predictive models, AI technology can lead to advancements in targeted therapies and individualized treatment plans. This is crucial for pediatric patients, as their developmental and physical needs are unique compared to adults. As such, AI’s ability to provide precise and actionable insights is likely to be game-changing.
In addition, the integration of AI tools in predicting glioma recurrence represents a proactive approach to patient care. Instead of merely reacting to recurrence after it happens, healthcare providers can identify at-risk patients early on, potentially preemptively addressing issues before they escalate. This strategic shift towards a more preventative model could significantly alter survival rates and quality of life for pediatric cancer patients, emphasizing the critical role of artificial intelligence in the future of oncology.
Clinical Trials: The Next Step for AI in Oncology
With the promising results obtained from current studies utilizing AI in the monitoring of pediatric gliomas, clinical trials represent the next pivotal step in assessing the effectiveness of these technologies in real-world settings. These trials will not only validate the AI’s predictive capabilities but also explore how these insights can be seamlessly integrated into existing treatment frameworks. Such integration could transform patient management by optimizing follow-up care and resource allocation.
As clinical trials progress, it is essential to consider the ethical implications and necessary safeguards for patient data privacy and healthcare equity. Ensuring that the benefits of AI advancements in cancer prediction are available to all populations will be crucial. By conducting diverse clinical trials that encompass a wide demographic cohort, researchers can establish comprehensive solutions that cater to the varied needs of pediatric cancer patients and their families across different communities.
Future Directions in Pediatric Brain Cancer Research
Looking ahead, the future of pediatric brain cancer research is poised for significant advancements, particularly with the integration of artificial intelligence and machine learning techniques. As researchers continue to explore the nuances of tumor biology and treatment responses, AI-driven analysis is expected to play an expanding role in unlocking new therapeutic avenues and enhancing predictive models. This multi-faceted approach may lead to breakthroughs not just in managing gliomas but also in understanding a broader spectrum of pediatric cancers.
Furthermore, fostering collaborations between technology companies and medical institutions will facilitate the continuous evolution of AI tools tailored for oncology. Such partnerships can lead to innovations in imaging, treatment protocols, and patient monitoring systems, ensuring that new findings translate into improved care for pediatric patients. Ultimately, the commitment to advancing research in pediatric brain cancer, grounded in the latest technological innovations, holds promise for better outcomes and a hopeful future for young patients battling this challenging disease.
Frequently Asked Questions
What is pediatric brain cancer and how does it relate to gliomas?
Pediatric brain cancer refers to tumors that develop in the brain of children. One common type of pediatric brain cancer is gliomas, which originate from glial cells in the brain. Although many pediatric gliomas can be treated successfully, predicting their recurrence remains challenging.
How can AI in cancer prediction improve outcomes for pediatric gliomas?
AI in cancer prediction utilizes advanced algorithms to analyze brain scans over time. In pediatric glioma cases, an AI tool was shown to enhance recurrence prediction accuracy, allowing for better-informed treatment decisions and potentially reducing unnecessary stress from frequent imaging for patients and families.
What advancements have been made in brain tumor treatment for children with gliomas?
Recent advancements in brain tumor treatment for pediatric patients include the use of AI technology that leverages temporal learning. This approach analyzes multiple MR scans over time, significantly improving the ability to predict glioma recurrence compared to traditional methods.
How does temporal learning in medicine benefit pediatric brain cancer patients?
Temporal learning in medicine helps by training AI models to recognize subtle changes in brain scans taken over months. This method, applied to predict pediatric glioma recurrence, achieves higher accuracy by utilizing longitudinal data, leading to potentially better patient outcomes.
What role does follow-up imaging play in managing pediatric brain cancer?
Follow-up imaging, such as MRI scans, is essential in managing pediatric brain cancer to monitor for recurrence. The traditional reliance on single scans for assessments poses challenges; however, AI-assisted techniques allow for improved risk stratification and can lead to less frequent imaging for low-risk patients.
What are the implications of AI predicting glioma recurrence in children?
The implications of AI predicting glioma recurrence are substantial. By utilizing advanced predictive models, clinicians can better identify high-risk patients for timely intervention, which could significantly enhance treatment outcomes and minimize the emotional and physical burden of frequent medical imaging.
How accurate are AI models in predicting glioma recurrence for pediatric patients?
AI models employing temporal learning demonstrated an accuracy rate of 75-89 percent in predicting glioma recurrence within a year post-treatment for pediatric patients, greatly surpassing the 50 percent accuracy of predictions made from single MR images.
What should families know about the treatment options for pediatric gliomas?
Families should know that treatment options for pediatric gliomas often include surgery, chemotherapy, and radiation therapy. The choice of treatment can depend on factors such as the tumor’s grade and location, as well as the child’s overall health, making accurate monitoring and risk prediction essential.
| Key Points | Details |
|---|---|
| AI Tool for Relapse Prediction | An AI tool predicts risk of relapse in pediatric brain cancer more accurately than traditional methods. |
| Focus on Pediatric Gliomas | The study primarily targets gliomas, tumors that can be treated effectively but have varying recurrence rates. |
| Temporal Learning Technique | The AI uses temporal learning to analyze multiple brain scans over months, improving prediction accuracy. |
| Accuracy of Predictions | The AI tool achieved 75-89% prediction accuracy, significantly better than the 50% accuracy of single image assessments. |
| Future Clinical Applications | Researchers aim to use this AI to improve care by reducing follow-up imaging or preemptively treating high-risk patients. |
Summary
Pediatric brain cancer, particularly gliomas, presents unique challenges for diagnosis and treatment. Recent advancements in AI technology have shown promising potential in predicting relapse risks in these pediatric patients. By employing a groundbreaking technique called temporal learning, researchers have demonstrated that combining insights from multiple brain scans can significantly enhance prediction accuracy. Moving forward, the integration of AI into clinical practices holds the promise of improving patient outcomes and reducing the burdens of frequent imaging for children recovering from brain tumors.